Area and 3-dimensional Volumetric Changes of Periapical Lesions after Root Canal Treatments
Wim Gerard van der Borden, DDS,* Xin Wang, MSD,† Min-Kai Wu, MSD, PhD,*and Hagay Shemesh, DDS, PhD*
From the *Department of Endodontology, Academic Center of Dentistry Amsterdam, University of Amsterdam and VU University, Amsterdam, The Netherlands; and †Department of Stomatology, Peking Union Medical College Hospital, Beijing, China.
Address requests for reprints to Dr Hagay Shemesh, Department of Endodontology, Academic Centre of Dentistry Amsterdam, University of Amsterdam and VU University, 1081 Amsterdam, The Netherlands. E-mail address: hshemesh@
acta.nl
0099-2399 – see front matter
Copyright ª 2013 American Association of Endodontists.https://dx.doi.org/10.1016/j.joen.2013.07.001
Abstract
Introduction: This study compared the changes insize of periapical lesions after rootcanal treatment as revealed by periapical radiography (PA) and cone-beam computed tomography (CBCT) imaging using area and 3-dimensional volumetric measurements and assessed the outcome of the treatments based on these parameters. Methods: Both PA and CBCT scans were taken preoperatively and at recall. In total, 50 teeth (71 roots) with evidence of periapical bone loss on both PA and CBCT images were endodontically treated and followed for 10–37 months. The area and volume of periapical lesions were measured, and changes were presented in the following 4 categories: lesion undetected, lesion reduced in size, lesion unchanged, or lesion enlarged. The McNemar and chi-square tests were used to compare the lesion changes determined by CBCT imaging and PA. Results: The 4-category diagnosis made using both methods were in agreement in 39 of 71 (54.9%) roots, where as disagreement was observed in 32 of 71 (45.1%) roots (P < .001). At recall, lesion was absent in 11 of 71 (15.5%) roots on CBCT scans and 32 of 71 (45.1%) roots on PA (P < .001). When success was defined as the absence of a lesion or a reduction in size of a lesion, 55 (77.5%) roots on CBCT imaging showed success and 63 (88.7%) roots on PA (P = .073). Conclusions: Changes in lesion size after root canal treatment determined with 3-dimensional volumetric CBCT data and 2dimensional PA data are different. The outcome of root canal treatments determined with PA could be untrue. (JEndod2013;39:1245–1249) Key Words
Cone-beam computed tomography, lesion changes, periapical radiography, volumetric measurements of
periapical lesions
- The whole lesion or part of it maybe within the cancellous bone and, thus, invisible on PA pretreatment (16) and/or at recall (10–12). When lesions enlarge or reduce in size within the cancellous bone or in a buccolingual direction, the change may be not assessable on PA (7). The size of periapical radiolucency on PA can be affected by the orientation of the film and tubehead. However, in most retrospective studies, the orientation of the preoperative radiographs was not registered (1), and the orientation of recall radiographs could be different, affecting the accuracy of assessing lesion changes. Because these changes determine the outcome, PA may be unreliable in assessing the outcome of root canal treatments.
- Recently, the accuracy of PA and cone-beam computed tomography (CBCT) imaging in diagnosing periapical lesions was assessed in several studies (8,17–20). CBCT imaging detected 20%–39% more posttreatment periapical lesions compared with PA (17–22). In a study by Velvart et al (23), all 78 CBCT-detected human periapical lesions, of which 17 were invisible on PA, were confirmed to be true bone defects during periapical surgery. Liang et al (8) examined 63 roots with artificial periapical bone defects and 37 roots without bone defects in human mandibles with PA and CBCT imaging; PA detected 42 (67%), whereas CBCT imaging detected 63 (100%) bone defects without any false-positives or false-negatives.Paula-Silva etal(6)evaluated the sensitivity, specificity, predictive values, and accuracy of PA and CBCT imaging in diagnosing apical periodontitis in dogs using histopathologic findings as a gold standard; the negative predictive value in diagnosing apical periodontitis was 0.46 for CBCT imaging and 0.25 for PA.
- However, neither PA nor CBCT images can distinguish scar healing from a periapical lesion. One may wonder whether CBCT overestimates the frequency of periapical lesions (24). Love and Firth (25) reported the histologic findings of 100 teeth with persistent post-treatment periapical radiolucency. A granuloma was diagnosed in 77 cases, a cyst in 18 cases, an abscess in 3 cases, and scar healing in 2 (2%) cases. Therefore, scar healing is a rare occurrence.
- CBCT imaging can be used to assess lesion changes after root canal treatment because it could provide volumetric data of periapical lesions. Mischkowski et al (26) found volumetric measurements in human maxilla to be accurate and reliable. Alhowalia et al (27) found that CBCT imaging is an accurate means of measuring the volume of artificially created bovine bone cavities in an ex vivo model. They further state that these volumetric measurements may provide a valuable tool for monitoring the healing rate of apical periodontitis. Their findings were verified later by Whyms et al (28). In a study by Liang et al (8), the physical volume of artificial periapical bone defects in human mandibles was measured. The volumes of bone defects measured with CBCT data and the values of the physical volumes were compared and were highly correlated (R2 =96.9%, P < .001). Although these in vitro studies confirm the reliability of volumetric measurements of periapical lesions on CBCTscans, noclinical studies sofar have used this method to determine the outcome of root canal treatments. The aim of this study was to measure the changes in lesion size after root canal treatments with PA and CBCT imaging and to assess the outcome based on these parameters.
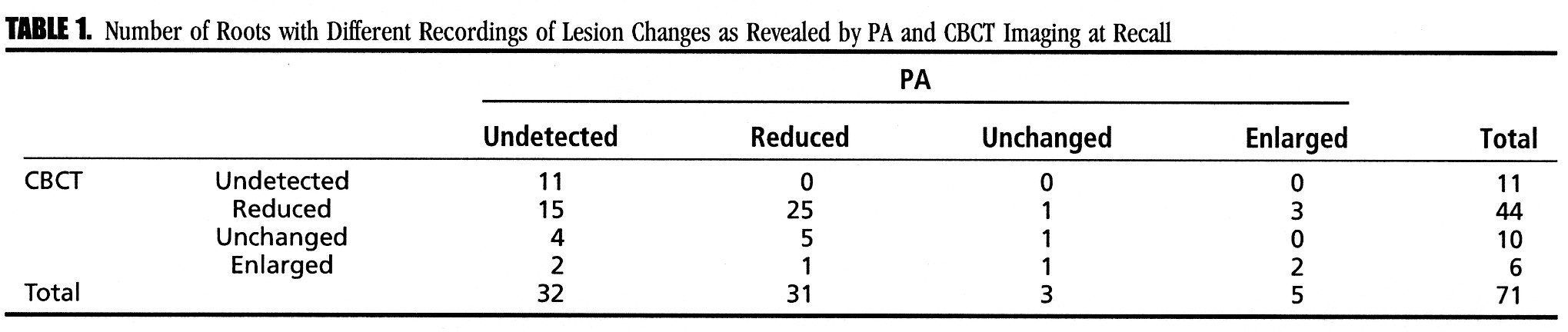
TABLE 1. Number of Roots with Different Recordings of Lesion Changes as Revealed by PA and CBCT Imaging at Recall
Materials and Methods
- In total,56 patients with at least 1 tooth presenting with a periapical lesion were treated by 1 operator (VDB) between October 2009 and May 2011. Forty-two of a total of 56 (75%) patients (32 women and 10 men, 21–78 years old) were followed for 10–37 months after treatment. They were informed of the aims and radiation dose of CBCTexamination, and their consent was secured. Thirty-one roots in 22 (2 premolars and 20 molars) teeth were excluded because they had no preoperative periapical radiolucency on PA, and, therefore, lesion reduction could not be assessed with the PA data. All selected roots showed preoperative periapical radiolucency on both PA and CBCT scans. In total, 71 roots (50 teeth including 9 anterior teeth, 6 premolars, and 35 molars) were included. Two roots in 1 patient were examined 10 months after treatment; the other 69 (97%) roots were examined 17–37 months after treatment.
- All root canal treatments, including initial treatments and retreatments, were performed in a single visit. The shaping, cleaning, and obturation procedures were described previously (29). Briefly, each tooth to be treated was isolated with a rubber dam. A dental operating microscope was used during treatment. The working length was determined by using Root ZX (J Morita Corp, Kyoto, Japan) and confirmed with PA. A crown-down technique with S-Apex nickel-titanium rotary instruments (FKG Dentaire, La Chaux-de-Fonds, Switzerland) was used to prepare all root canals. The apical portion of the root canal was enlarged to at least #60 depending on the root canal morphology. Irrigation with 3% hydrogen peroxide solution and 2% sodium hypochlorite solution was performed after each file. After completion of instrumentation, additional passive ultrasonic irrigation was performed with 2% sodium hypochlorite solution and 17% EDTA using a P MAX device (Satelec, Meriganc Cedex, France). Root canals were dried and filled with gutta-percha cones and AH26 sealer (Dentsply DeTrey GmbH, Konstanz, Germany) using lateral compaction and later warm vertical compaction techniques. A System B heat source with a 30/0.04 plugger (Analytic Technology, Redmond, WA) was used to down-pack the gutta-percha in the canal. Backfill was achieved by using an Obtura II unit (Obtura Corporation, Fenton, MO). The pulp chamber was filled with PhotoCore (Kuraray, Osaka, Japan), and the coronal restoration with Clearfil AP-X Composite (Kuraray) was placed immediately after root canal treatment.
- Preoperatively and at recall, straight projection intraoral PAs were obtained with a dental X-ray machine Kodak RVG6100 (Carestream Dental LLC, Atlanta, GA) using a parallel technique. The exposure parameterswere65kV,7.5mA,and0.15 seconds.CBCTscans(Gendex CB-500; KaVo Dental GmbH, Biberach, Germany) with exposure parameters of 120 kV, 5 mA, and 6–11 seconds were taken of the area of interest. All CBCT scans were reformatted with 0.125–0.2 slice intervals and 1.5-mm slice thickness.
- The lesion area on PA was measured in square millimeters using ImageJ 1.28 software (National Institutes of Health, Bethesda, MD) as previously described (6). Freehand selection was used to trace out the border of the lesion and then measure and record the area value. Measurements of lesion volume on CBCT data in Digital Imaging and Communication in Medicine format was performed using Amira 5.4.3 (Visage Imaging GmbH, Berlin Germany) software. A local thresholddetermining algorithm (8, 30) with a manual tracing intervention was used to plot out the border of the lesion (8). After setting the threshold, the border of lesion was determined by the computer automatically. Modifications of the border were performed with the ‘‘brush’’ function, and then the 3D volume was measured and recorded.
- The outcome was presented in 4 categories: lesion undetected, reduced in size, unchanged, and enlarged. A periapical lesion was defined as radiolucency associated with the radiographic apex of the root, which was at least twice the width of the periodontal ligament space (18). Reduced and enlarged lesions were determined when the area or volume of radiolucency had reduced or enlarged by 20% or more (8). An unchanged lesion was defined as a lesion change less than 20%. All the PA and CBCT images were pooled and blindly assessed twice by 1 operator who was not involved in the treatments. There was a 2-week interval between the 2 assessments.
- The Cohen kappa coefficient was used to assess the intraobserver agreement of the radiographic assessments. The McNemar and chisquare tests were used to compare the outcome determined by CBCT imaging and PA.The statisticalanalyseswere performedusing SPSS software (version 15.0; SPSS Inc, Chicago, IL). The level of significance was set at alpha = 0.05.
Results
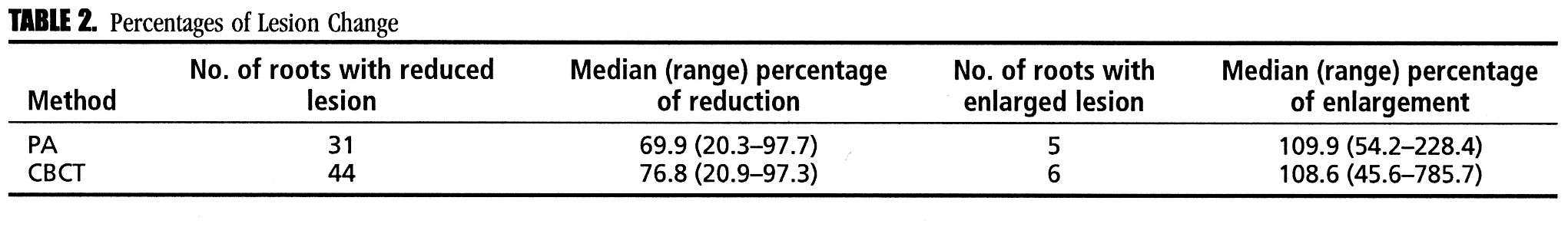
TABLE 2. Percentages of Lesion Change
- The repeated assessment of radiographs and CBCT scans by 1 examiner resulted in an intraexaminer agreement of 0.75 and 0.76
(Cohen kappa), respectively. The lesion changes revealed by PA and CBCT imaging are shown in Table 1. The findings determined by PA significantly differed from those by CBCT imaging (P < .001). In 39 of 71 (54.9%) roots, the 4-category diagnosis resulted from both methods was in agreement, whereas disagreement was observed in 32 of 71 (45.1%)roots (Table 1). The percentage of undetected lesions determined with CBCT scans (15.5%) was significantly lower than that by PA (45.1%) (P < .001). However, the percentages of undetected and reduced lesions together as revealed by CBCT imaging (77.5%) and PA (88.7%) were not significantly different (P = .073). Sixty-three roots showed radiographic healing (either undetected or reduced lesions) on PA; the healing tendency of 55 of 63 (87%) roots was confirmed by CBCT imaging (Table 1). - The preoperative periapical radiolucencies varied from 0.3 mm2 to 61.7 mm2 (median = 4.7 mm2) on PA and 1.0 mm3 to 281.5 mm3 (median = 22.9 mm3) on CBCT imaging. The percentages of lesion changes after treatments are shown in Table 2 and Figure 1A–D.
Discussion
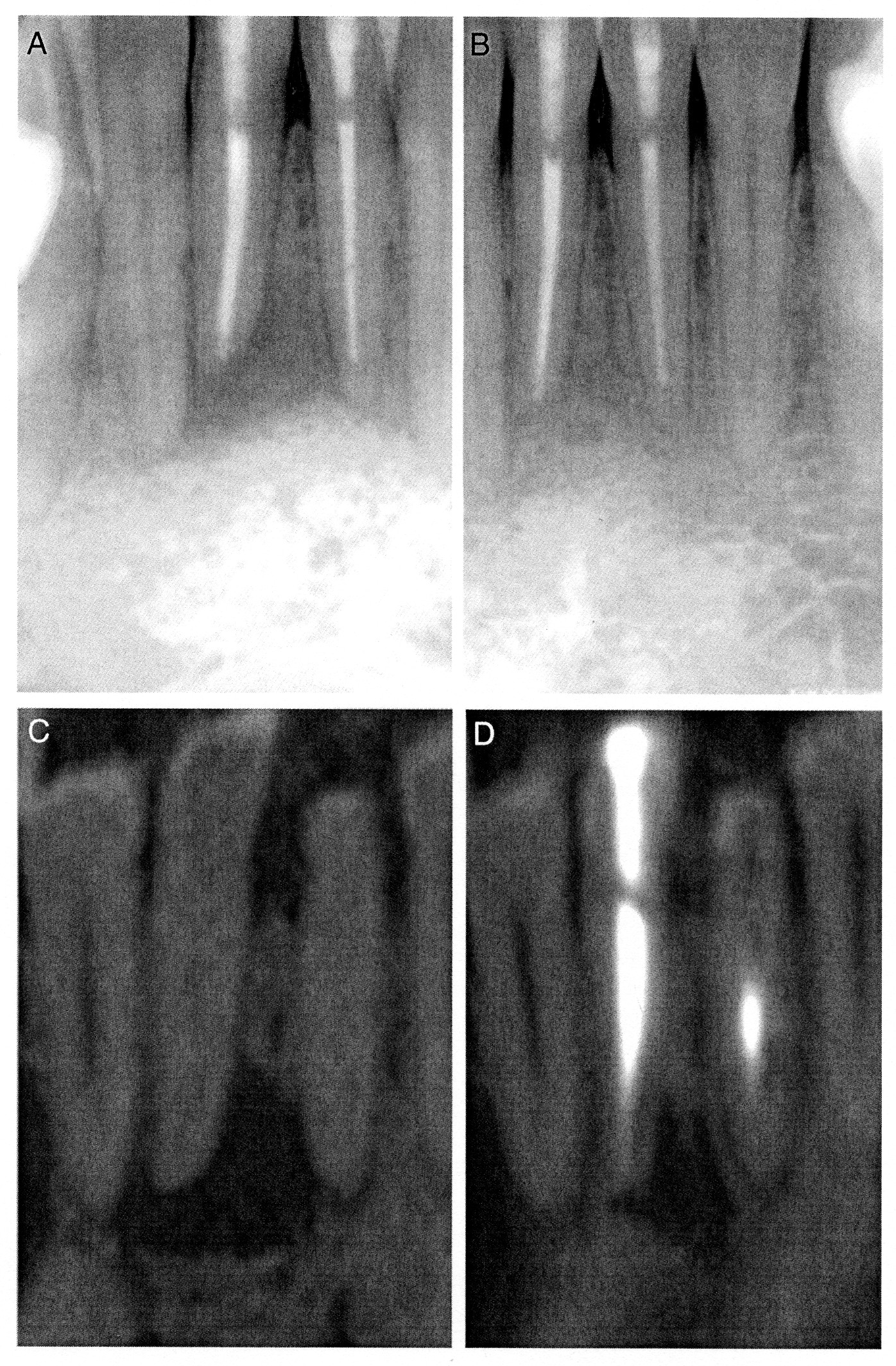
Figure 1. (A and B) Pre- and post-treatment radiographs of tooth 41; a lesion was not detected post-treatment. C and D are the pre- and post-treatment CBCT images of the same tooth; post-treatment periapical radiolucency was present, and the volume of radiolucency reduced by 63.8%.
- To our knowledge, this is the first study in which the volumes of lesions before and after root canal treatment were measured, and the changes in size were determined with 3D volumetric data. One observer performed all area and volumetric measurements with PA and CBCT data twice, and the measurements were reproducible; intraexaminer agreement was determined as a Cohen kappa of 0.75 and 0.76, respectively.
- CBCT detected post-treatment periapical radiolucency in 21 of 32 roots that did not show radiolucencies on PA (Table 1). Because no histologic evaluation was attempted, the reliability of radiographic diagnosis is unknown. However, because no CBCT false-positives were found in previous studies on the accuracy of CBCT imaging in diagnosing periapical lesions (6, 8, 20, 23, 31), the 21 lesions detected by CBCT only are most likely to be true post-treatment lesions. This indicates that PA could overestimate the percentage of teeth without posttreatment periapical radiolucency. The majority of these 21 lesions decreased in size after root canal treatment as confirmed by CBCT imaging (Fig. 1).
- On 1 root,a lesion was reduced insize on PA but enlarged on CBCT imaging; in 3 roots, lesions were enlarged on PA but reduced on CBCT scans (Table 1). Paula-Silva et al (7) concluded that size changes could bemisinterpretedwithPA.Similartootherretrospectivestudies(1),the orientation of the preoperative radiographs was not registered in this study; a different orientation at recall could affect the diagnosis of lesion changes and lead to erroneous outcome determination. Furthermore, part of the lesion could be in the cancellous bone and, therefore, invisible on PA or the lesion enlarged or reduced in the buccolingual direction. In these cases, changes in lesion size could only be measured with CBCT data (7).
- In total, CBCT imaging detected 44 roots with lesion reduction, whereas PA detected 31 roots only. Fifteenof 44 CBCT-detected reduced lesions were invisible on radiographs at recall (Table 1). Because many periapical lesions are invisible on PA pretreatment and at recall, the change in size of these lesions after treatment is not always assessable with PA. This explains why PA detected more roots without lesions but fewer roots with reduced lesions than CBCT imaging (Table 1). The absence of periapical radiolucency indicates the absence of periapical bone defect but does not guarantee the absence of periapical inflammation (6, 13). Either the absence of a lesion or a reduction in its size suggests periapical healing (1). In the present study, 63 roots showed radiographic healing on PA; 87% of them were confirmed as such by CBCT imaging (Table 1). However, more clinical studies are needed to verify this trend and to determine whether PA can reliably assess the reduction in size of lesions (1).
- In this study, all 71 roots showed preoperative periapical radiolucency on both CBCT imaging and PA. Therefore, the change in lesion size after treatment could be observed with both PA and CBCT data. Some teeth in this study had roots without preoperative periapical radiolucencies on PA. These roots were not included in the experiment because they might show evidence of periapical bone loss on CBCT imaging, but their lesion reduction was not assessable with the PA data. A lesion was absent in 32 of 71 (45.1%) roots on PA (Table 1). This percentage is lower than those reported previously (1) partly because the follow-up period in this study was 10–37 months. A number of studies (32–35) reported high success rates in which success was defined as a periapical index (PAI) scores of 1 and 2 (33, 34). However, PAI score of 2 represents a small periapical bone defect and mild inflammation (32, 36). When only a PAI score of 1 (ie, the absence of periapical radiolucency) would be considered as ‘‘success,’’ the success rate for teeth with preoperative periapical lesion would drop from 79% to 26% (33).
The disadvantages of CBCT imaging are higher cost and a potentially higher radiation dose. In this study, Gendex CB-500 was used to make CBCT scans; a small field of view that reduces the radiation dose (24) was not available. A number of factors may influence the outcome including the detailed anatomy of root canals in premolars and molars, the apical extension and quality of root fillings, and initial root canal treatment or retreatment (2). The effects of such potential influencing factors on outcome should be tested in future studies with a large sample size and multivariate logistic regression analysis. The purpose of this study focused on the comparison of outcome determined with PA and CBCT imaging. With the findings of this study, we concluded that lesion changes after root canal treatments determined with 3D volumetric CBCT data and 2-dimensional PA data were different, and, thus, the outcome determined with PA could be untrue.
Acknowledgments
The authors deny any conflicts of interest related to this study.
References
- Ng Y-L, Mann V, Rahbaran S, et al. Outcome of primary root canal treatment: systematic review of the literature—part 1. Effects of study characteristics on probability of success. Int Endod J 2007;40:921–39.
- Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto Study. Phase 1: initial treatment. J Endod 2003;29:787–93.
- Kirkevang L-L, Hørsted-Bindlev P. Technical aspects of treatment in relation to treatment outcomes. Endod Topics 2002;2:89–102.
- Friedman S. Considerations and concepts of case selection in the management of post-treatment endodontic disease (treatment failure). Endod Topics 2002;1: 54–78.
- Huumonen S, Ørstavik D. Radiological aspects of apical periodontitis. Endod Topics 2002;1:3–25.
- Paula-Silva FWG, Wu M-K, Leonardo MR, et al. Accuracy of periapical radiography and cone beam computed tomography in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod 2009;35:1009–12.
- Paula-Silva FWG, Hassam B, da Silva LAD, et al. Outcome of root canal treatment in dogs determined by periapical radiography and cone-beam computed tomography scans. J Endod 2009;35:723–6.
- Liang Y-H, Jiang L, Gao X-J, et al. The ability of cone-beam computed tomography to determine the presence and size of artificial periapical lesions in human mandibles. Int Endod J 2013 June 7 [Epub ahead of print].
- Patel S, Wilson R, Dawood A, et al. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography—part 1: preoperative status. Int Endod J 2012;45:711–23.
- Bender IB, Seltzer S. Roentgenographic and direct observation of experimental lesions in bone: I. J Am Dent Assoc 1961;62:152–60.
- Stabholz A, Friedman S, Tamse A. Endodontic failures and re-treatment. In: Cohen S, Burns RC, eds. Pathways of the Pulp, 6th ed. St Louis, MO: Mosby; 1994:692–3.
- Ricucci D, Bergenholtz G. Bacterial status in root-filled teeth exposed to the oral environment by loss of restoration and fracture or caries—a histobacteriological study of treated cases. Int Endod J 2003;36:787–802.
- Brynolf I. A histological and roentgenological study of periapical region of human upper incisors. Odontol Revy 1967;18(Suppl 11):1–97.
- Barthel CR, Zimmer S, Trope M. Relationship of radiologic and histologic signs of inflammation in human root-filled teeth. J Endod 2004;30:75–9.
- Wu M-K, Dummer PMH, Wesselink PR. Consequences of and strategies to deal with residual post-treatment root canal infection. Int Endod J 2006;39:343–56.
- Patel S, Wilson R, Dawood A, et al. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography—part 2: a 1-year post-treatment follow-up. Int Endod J 2012;45:711–23.
- Lofthag-Hansen S, Huumonen S, Gr€ondahl K, et al. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:114–9.
- Low KM, Dula K, B€urgin W, et al. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod 2008;34:557–62.
- Estrela C, Bueno MR, Leles CR, et al. Accuracy of cone beam computed tomography, panoramic and periapical radiographic for detection of apical periodontitis. J Endod 2008;34:273–9.
- Cheung GS, Wei WL, McGrath C. Agreement between periapical radiographs and cone-beam computed tomography for assessment of periapical status of root filled molar teeth. Int Endod J 2013 Feb 5 [Epub ahead of print].
- Christiansen R, Kirkevang L-L, Gotfredsen E, et al. Periapical radiography and cone beam computed tomography for assessment of the periapical bone defect 1 week and 12 months after root-end resection. Dentomaxillofac Radiol 2009;38:531–6.
- Moura MS, Guedes OA, Alencar AH, et al. Influence of length of root canal obturation on apical periodontitis detected by periapical radiography and cone beam computed tomography. J Endod 2009;35:805–9.
- Velvart P, Hecker H, Tillinger G. Detection of the apical lesion and mandibular canal in conventional radio- graphy and computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:682–8.
- Petersson A, Axelsson S, Davidson T, et al. Radiological diagnosis of periapical bone tissue lesions in endodontics: a systematic review. Int Endod J 2012;45:783–801.
- Love RM, Firth N. Histopathological profile of surgically removed persistent periapical radiolucent lesions of endodontic origin. Int Endod J 2009;42:198–202.
- Mischkowski RA, Pulsfort R, Ritter L, et al. Geometric accuracy of a newly developed cone-beam device for maxillofacial imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;104:551–9.
- Ahlowalia MS, Patel S, Anwar HMS. Accuracy of CBCT for volumetric mesurement of simulated periapical lesions. Int Endod J 2013;46:538–46.
- Whyms BJ, Vorperian HK, Gentry LR, et al. The effect of computed tomographic scanner parameters and 3-dimensional volume rendering techniques on the accuracy of linear, angular, and volumetric measurements of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:682–91.
- Ven der Borden WG, Wu M-K, Wesselink PR. Percentages of gutta-percha–filled canal area observed after increased apical enlargement. J Endod 2010;36:139–42.
- Chang PC, Liang K, Lim JC, et al. A comparison of the thresholding strategies of micro-CT for periodontal bone loss: a pilot study. Dent Maxillofac Radiol 2013; 42:66925194.
- Patel S, Dawood A, Mannocci F, et al. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J 2009;42:507–15.
- Ørstavik D, Kerekes K, Eriksem HM. Clinical performance of three endodontic sealers. Endod Dent Traumatol 1987;3:178–86.
- Ørstavik D, Qvist V, Stoltze K. A multivariate analysis of the outcome of endodontic treatment. Eur J Oral Sci 2004;112:224–30.
- Marquis VL, Dao T, Farzaneh M, et al. Treatment outcome in endodontics: the Toronto Study—phase III: initial treatment. J Endod 2006;32:299–306.
- Waltimo TMT, Boiesen J, Eriksen HM, et al. Clinical performance of 3 endodontic sealers. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:89–92.
- Wu M-K, Shemesh H, Wesselink PR. Limitations of previously published systematic reviews evaluating the outcome of endodontic treatment. Int Endod J 2009;42: 656–66.





















